Introduction:
Myelodysplastic syndrome (MDS) is a diverse group of hematological malignancies characterized by dysfunctional pluripotent stem cells, leading to abnormal hematopoiesis and cytopenia. Early diagnosis is crucial for improving patient outcomes. Artificial Intelligence (AI) and Machine Learning (ML) have emerged as powerful tools in healthcare for disease diagnosis and monitoring. This review aims to summarize the current state of AI application in the diagnosis of MDS, discussing various ML models, their advantages, disadvantages, and performance metrics.
Methods:
A comprehensive search strategy was developed using Medical Subject Headings (MeSH) terms and relevant keywords related to MDS and AI/ML. Pubmed, Embase, and scopus were searched, and duplicates were removed. Only original research articles studying ML algorithms in the diagnosis of MDS in human subjects were included. Studies on animals, reviews, non-original articles, and non-English papers were excluded. For each article, data on the area under the receiver operating curve, sensitivity, specificity, and accuracy for the best preforming model were collected.
Results:
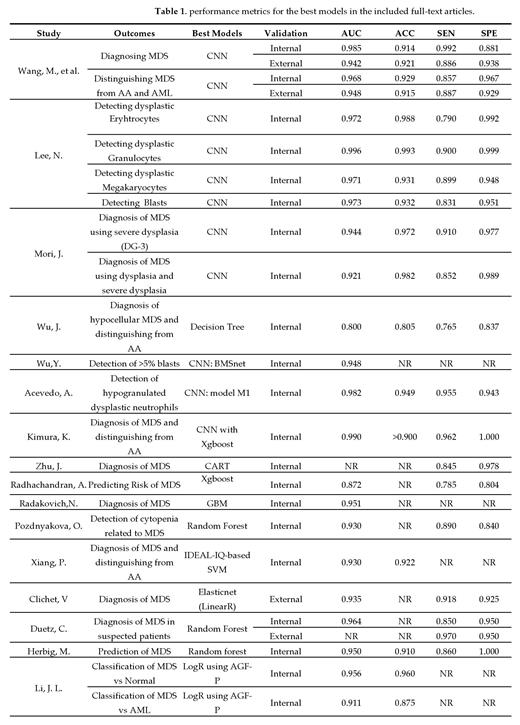
The search yielded 313 articles, and after screening, 16 articles met the inclusion criteria. These articles were grouped based on the data utilized in the training of their models. Five articles utilized bone marrow smears for the training of their data. Their models aimed to detect dysplastic cells and blasts in bone marrow smears. The majority of these studies utilized convolutional neural network (CNN), a ML algorithm, for image recognition. One study utilized decision tree models. The AUC of these models ranged between 0.8 and 0.996. All the models were internally validated but were not externally validates. Three studies utilized peripheral blood smears for the training of their ML models. Two of these studies also utilized CNN for the detection of dysplasia and subsequent diagnosis of MDS. One study utilized CART to create a decision tree algorithm. The AUC for these models ranged between 0.982-0.99. Four studies utilized flowcytometry data from bone marrow samples for the training of their AI models. These models achieved AUC ranging between 0.935-0.97. Two of these models were both internally and externally validated, one of which was on a prospective cohort.
Conclusion:
The integration of AI and ML in MDS diagnosis holds promise for early detection and improved patient care. The reviewed studies showed encouraging results, indicating that AI-based approaches can complement traditional diagnostic methods and aid in making more informed clinical decisions especially when it comes to analysing blood/bone smears. However, many of these models need to be externally validated in large prospective cohorts to establish AI's role in routine clinical practice.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal